Abstract
Background
Limited research had explored health care utilization (HCU) in transitioning adolescent/young adults (AYAs) with sickle cell disease (SCD). Major limitations of the current studies include the use of cross-sectional designs and lack of longitudinal exploration of HCU trajectories and the factors that might contribute to the increased HCU. The purposes of this longitudinal database study were to describe HCU trajectories of transitioning AYAs with SCD and examine factors associated with these trajectories.
Methods
AYAs (12-27 years) at one urban center with a comprehensive SCD program were included if they had SCD (SS, SC, Sβ+, Sβ° genotypes) and at least two pediatric SCD clinic encounters between 01/01/1989 and 07/30/2015. We used latent class growth modeling to identify HCU (clinic, Emergency department (ED), hospitalizations) trajectories and ordinal logistic regression to examine factors associated with HCU, including individual (demographic; disease measures including severity, comorbidities, and medications), contextual (distance to clinic), and transfer-related factors (transfer age and continuity of care). We also calculated age-related ED reliance (EDR)scores. Significance was set at p<0.05.
Results
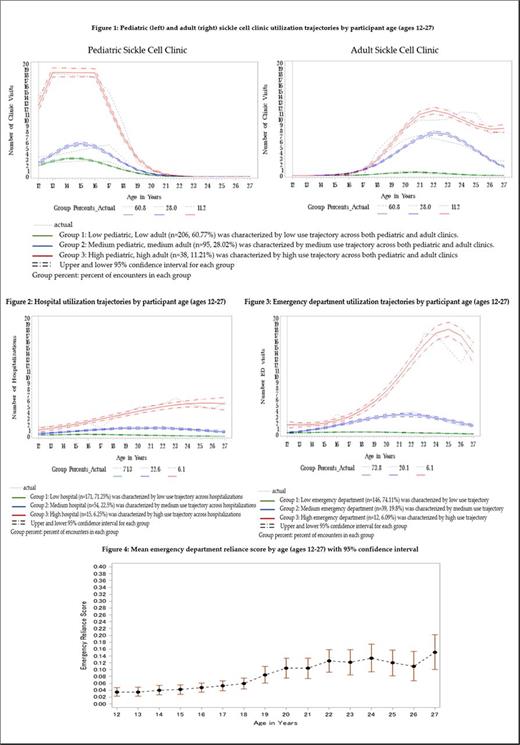
339 AYAs (55% male; 96% black; mean age=24.5 years, SD=5.38) had 10848 clinic encounters. Of these, 240 AYAs (71%) had 3840 hospitalizations and 197 (58%) had 3152 ED encounters. Low, medium, and high utilization groups were identified, with the majority of AYAs having low clinic (n=206, 60.77%), low hospital (n=171, 71.25%), and/or low ED (n=146, 74.11%) utilization trajectories (Figures 1-3). Mean age-related EDR scores were < 0.33 and increased with age (figure 4). AYAs transferred at mean age 19 and the majority had at least one additional adult clinic encounter.
Factors significantly associated with higher clinic utilization trajectories included iron overload (OR=36.6; p <0.0001; 95% CI= 11.657-114.979), lower extremity ulcers (OR=8.5; p= 0.0174; 95% CI=1.457- 49.906), cerebral infarct/vasculopathy (OR=7.2; p <0.0001; 95% CI= 3.599-14.51), hydroxyurea (OR=3.2; p= 0.0007; 95% CI= 1.626-6.198), attention deficit disorders (OR=11.5; p= 0.0003; 95% CI= 3.033-43.505), and distance to clinic (OR=0.98; p <0.0001; 95%CI= 0.970-0.989).
Factors significantly associated with higher hospitalization trajecotries included chronic pain (OR=3.3; p <0.0001; 95% CI=1.916-5.522), long-acting narcotics (OR=2.3; p= 0.0254; 95% CI= 1.11- 4.933), hydroxyurea (OR= 1.9; p= 0.0343; 95% CI= 1.047-3.341), intellectual disabilities (OR=7.96; p= 0.0129; 95% CI=1.551-40.858), and depression (OR=2.2; p= 0.0180; 95% CI= 1.146- 4.271).
Factors significantly associated with higher ED utilization trajectories included hip/shoulder avascular necrosis (OR=28.9; p <.0001; 95% CI=5.921-140.731), long-acting narcotics (OR=32.5; p <0.0001; 95% CI=7.717-136.927), major depression (OR=22.5; p <0.0001; 95% CI= 4.952-102.591), and distance to clinic (OR=0.95; p <0.0001; 95% CI=0.923-0.974).
SCD genotype and SCD severity scores were not associated with group membership in any of the HCU trajectories.
Conclusions
Different factors were associated with different HCU trajectories, underscoring the complexity of HCU during transition. Understanding the factors associated with HCU might help identify AYAs with SCD at risk for high utilization.
Shah: Alexion: Other: Speaker; Novartis: Other: Speaker.
Author notes
Asterisk with author names denotes non-ASH members.